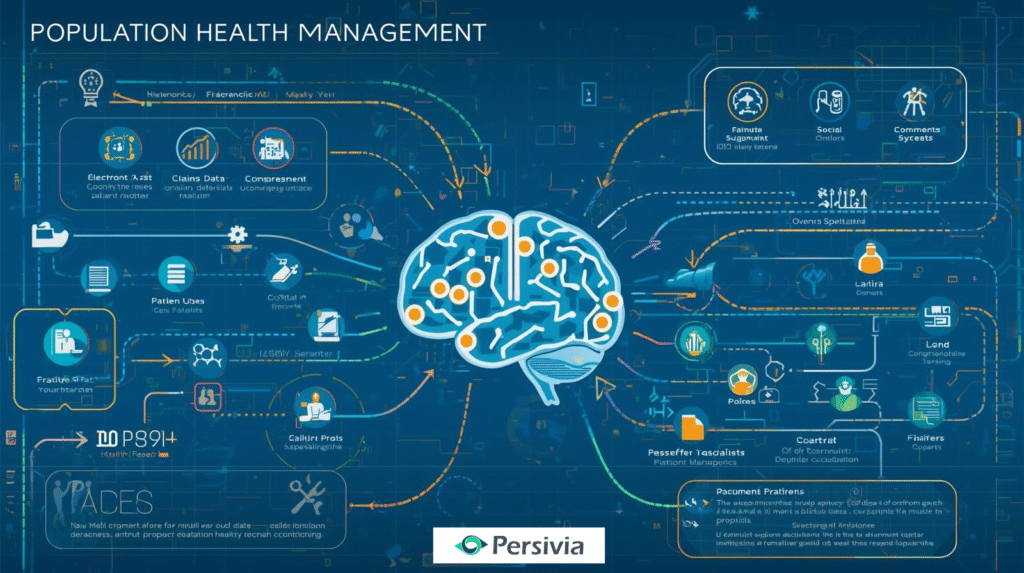
Population Health Management Platforms help healthcare organizations improve equity and access by integrating EMR, claims, and social data into full patient profiles. AI-driven analytics identify vulnerable groups early, while care coordination tools connect them with the right specialists and resources. These platforms support proactive outreach to underserved populations and align with value-based care models, ensuring providers focus on outcomes rather than volume.
Millions of people in communities all over the world are impacted by healthcare disparities. Rural and urban centers do not have specialists. The former are overcrowded, and the vulnerable people cannot get care in time due to the barriers they encounter. The answer is to use technology to uncover gaps, anticipate needs, and pull resources together.
A Population Health Management Platform provides the fundamental framework for managing these issues systematically. These platforms combine information provided by several sources, process trends based on demographic factors, and allow healthcare institutions to plan specific interventions. Instead of managing symptoms when they occur, the method aims at preventing health concerns and providing equal access to care to every member of society.
Understanding Healthcare Equity Through Data
Healthcare equity refers to the fact that all individuals can get the right care irrespective of their location, income, race, or social status. Natural health care systems tend to exclude those populations that are vulnerable and require care the most.
Modern platforms reverse this dynamic by gathering data that reveals patterns behind the scenes. They combine electronic health records, insurance claims, social services, and community resources with information to develop complete patient profiles.
The Role of Social Determinants
Social determinants significantly impact health outcomes across different populations. Population Health Management analytics examine factors like:
- Housing stability and neighborhood safety
- Access to transportation and healthy food
- Employment status and insurance coverage
- Educational attainment and health literacy
- Language barriers and cultural preferences
Such insights can assist healthcare teams in comprehending the factors that lead to poorer outcomes in some groups and developing relevant interventions.
Identifying At-Risk Populations
Advanced platforms have a predictive model that identifies people at risk of developing chronic conditions or having a health crisis. This is proactive, where there are early interventions being undertaken to avoid expensive emergencies.
Risk stratification algorithms process several data points to classify patients based on their risk of hospitalization, medication non-adherence, or care gaps. Healthcare teams can then focus on areas of outreach in which they will create the most impact.
Breaking Down Access Barriers
Large populations are unable to receive proper healthcare services due to geographic barriers, financial limitations, and institutional obstacles. Through technological platforms, these issues are solved by coming up with creative solutions that bring care to the patients directly.
Expanding Care Reach
Integration of telemedicine helps specialists to provide service to remote groups of people without the need to travel long distances by the patient. The population health management tools organize virtual consultations and ensure the continuity of care between multiple providers.
Care teams can find patients who could use remote monitoring programs and supply the devices needed and detailed training plans. This is especially effective in chronic health conditions like diabetes, hypertension, and cardiovascular disease.
Coordinating Community Resources
Extensive networks unite medical care players with the local agencies that fuel basic human social requirements. Integrated systems automatically create referrals to the relevant social service agencies when patients face food insecurity or housing instability.
- Food assistance programs and nutrition counseling services
- Transportation support and medical ride coordination
- Housing assistance and utility payment programs
- Employment training and educational advancement resources
- Mental health counseling and addiction treatment services
This is a holistic method of considering health outcomes as factors that go far beyond clinical interventions.
Integrating AI for Personalized Care
Artificial intelligence changes the way in which healthcare organizations define needs and provide interventions. Machine learning programs process large quantities of information to pick out patterns that a human analyst may overlook.
Predictive Analytics in Action
The systems that run on AI can be used to estimate which patients are the most likely to attend the appointment, miss their medications, or develop complications. This helps healthcare teams to take the initiative and reach out to them on a personal basis.
Such as Patients who have a record of non-adherence to medications may receive automatic reminders, pharmacy appointments, or regulated dosing schedules. At-risk individuals may be linked with mental health resources before the development of severe symptoms of depression.
Automating Care Coordination
The digital health platform can also be used to offer more than just data analysis, but rather automated workflow processes that guarantee patients get the right follow-up care. The system may automatically make appointments, request more tests, or give care managers notification when the laboratory findings suggest a problem.
This automation helps to ease the load on the administrative staff of healthcare facilities and prevents the fall of a patient into the cracks. It is especially useful when dealing with a large population of patients with various needs.
Evidence-Based Care Pathways
AI systems use clinical guidelines and best practices to suggest the most effective treatment options in various groups of patients. The following evidence-based pathways can be used to ensure that every patient receives high-quality care, irrespective of the provider they visit.
Care pathways can be customized based on patient characteristics, preferences, and social circumstances to maximize effectiveness and adherence.
Data Integration and Interoperability
Effective population health management is impossible without a smooth flow of data between various healthcare systems and community organizations. New systems are good at integrating disparate data sources to form cohesive patient records.
Comprehensive Data Sources
Effective interfaces combine data between touchpoints in the healthcare ecosystem:
| Data Source | Information Type | Impact on Equity |
| Electronic Health Records | Clinical data, diagnoses, and treatments | Identifies care gaps and treatment patterns |
| Insurance Claims | Utilization patterns, costs, outcomes | Reveals access barriers and resource allocation |
| Social Services | Housing, nutrition, and employment status | Addresses social determinants of health |
| Community Organizations | Program participation, resource usage | Coordinates comprehensive support services |
| Health Information Exchanges | Care coordination, specialist referrals | Prevents duplicate testing and ensures continuity |
Breaking Down Data Silos
The healthcare organizations are usually faced with a disjointed, poorly communicating data system. An advanced platform eliminates this challenge by providing unified views of patient information accessible to all authorized personnel in the team.
Interoperability is also essential to support vulnerable groups of people who can be served by various providers and organizations. The coordination of care is enhanced when all people have access to all the information about patients.
Measuring Impact and Outcomes
Monitoring achievement of equity objectives needs powerful analytics and reporting tools. Platforms should have a history of improving access, quality, and outcomes in relation to various groups of the population.
Key Performance Indicators
Healthcare organizations use specific metrics to assess their progress toward equity goals:
- Access Metrics: Time to appointment, geographic coverage, specialist availability
- Quality Measures: Preventive care rates, chronic disease management, patient satisfaction
- Outcome Indicators: Hospital readmissions, emergency department visits, medication adherence
- Equity Assessments: Outcome disparities between different demographic groups
Continuous Improvement
Evidence-based knowledge allows healthcare institutions to develop their strategies over time. Teams can scale effective strategies and adapt less effective ones when some interventions are found to be more effective when applied to specific populations.
Frequent analysis will enable it to recognize new equity challenges as they arise and develop strategies to respond. This cycle method makes population health programs sensitive to the evolving community needs.
Implementation Strategies
Implementation of population health management technology will need thorough planning and stakeholder involvement to successfully roll out the technology. Organizations need to look at technical requirements, workflow integration, and change management.
Building Cross-Sector Partnerships
Addressing health equity requires collaboration between healthcare providers, social services, community organizations, and government agencies. Platforms facilitate these partnerships by enabling secure data sharing and coordinated service delivery.
Successful implementations often include:
- Healthcare systems and primary care practices
- Public health departments and social services
- Community-based organizations and nonprofits
- Educational institutions and employers
- Transportation and housing agencies
Staff Training and Adoption
Technology can only be useful when healthcare teams know how to utilize it appropriately. Extensive training initiatives can enable personnel to capitalize on the benefits of Population Health Management analytics to enhance patient care.
Data interpretation, workflow integration, and strategies to engage the patient should be trained. Constant reinforcement means that the teams will keep improving their skills as the platforms keep changing.
The Path Ahead
Population Health Management Platform technology offers unprecedented opportunities to address healthcare disparities and improve access for underserved communities. By integrating extensive data, providing AI-driven analytics, and aligning care delivery, these platforms can help healthcare organizations identify what is needed proactively and provide specific interventions that can make a tangible impact in the lives of people.
Persivia provides the latest population health management platforms, which transform data into actionable insights to achieve improved health results. Persivia’s CareSpace® is an AI-driven system that seamlessly integrates with more than 70 EMR systems and manages over 100 million patient records, providing the full analytics and care coordination capabilities your organization requires to eradicate health inequities.