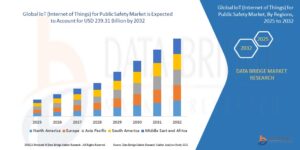
In the healthcare industry, risk adjustment models use statistical methods to examine medical problems and demographics in order to anticipate patient expenses. The three primary systems are HHS-HCC (ACA marketplace), CMS-HCC (Medicare Advantage), and CDPS (Medicaid). While providing patients with the right care, these models translate medical complexity into risk ratings and determine payment changes that guarantee healthcare organizations’ financial viability.
There is no universal trend in healthcare prices. The resources required by a 25-year-old marathon runner and an 85-year-old with heart disease and diabetes are different. By forecasting each patient’s medical expenses according to their unique details, risk adjustment models in healthcare industry provide a just payment structure that maintains the financial stability of the whole healthcare system.
These statistical models convert clinical complexity into numerical scores that drive billions of dollars in healthcare payments. Understanding patient risk levels enables government programs, insurance companies, and hospitals to manage resources efficiently, preserve financial stability, and guarantee that high-quality care reaches the people who need it most.
What Are Risk Adjustment Models?
Risk adjustment models are statistical forecasting systems that predict healthcare costs for individuals based on their unique characteristics.
These models function as financial planning tools that consider multiple factors:
- Age and demographic information
- Medical history and existing conditions
- Previous healthcare utilization patterns
- Prescription medication needs
- Social determinants of health
Healthcare organizations use these predictions to set appropriate payment rates, allocate resources, and maintain financial stability across different patient populations.
Three Primary Risk Adjustment Systems
Healthcare operates through three distinct risk adjustment frameworks, each serving different market segments and patient populations.
CMS-HCC Model: Medicare’s Foundation
The Centers for Medicare & Medicaid Services Hierarchical Condition Categories model targets Medicare Advantage programs specifically.
This system underwent major updates in 2024:
- Expansion from 86 to 115 distinct condition categories
- Comprehensive remapping of diagnostic codes
- Refined payment calculations resulted in a 3.56% average decrease in payments
- Enhanced accuracy for chronic condition management
The CMS-HCC model focuses on prospective risk adjustment, using previous year diagnoses to predict current year costs.
CDPS System: Medicaid’s Approach
The Chronic Illness and Disability Payment System addresses Medicaid beneficiaries’ unique healthcare needs.
CDPS excels in evaluating specific populations:
- Low-income families requiring comprehensive care
- Children with specialized medical needs
- Pregnant women needing obstetric services
- Elderly individuals with multiple conditions
- People with disabilities requiring ongoing support
The enhanced CDPS+Rx version incorporates prescription data, creating more accurate risk assessments for complex patient needs.
HHS-HCC Model: ACA Marketplace Solution
The Health and Human Services Hierarchical Condition Categories model serves the Affordable Care Act marketplace.
Key distinctions include:
- Current-period diagnosis evaluation
- Coverage across all age groups
- Specialized high-risk obstetric categories
- Real-time risk adjustment capabilities
This model helps balance costs between insurance plans, making coverage affordable for individuals with higher health needs.
How RAF Scoring Works
Risk Adjustment Factor scoring converts medical complexity into numerical values through a systematic four-step process.
Step 1: Diagnosis Coding
Medical practitioners use standardized ICD-10-CM codes to record patient conditions. These codes create a thorough medical profile by capturing everything from acute illnesses to chronic ailments.
Step 2: Risk Category Mapping
Diagnostic codes map to specific risk categories within each model. Similar conditions group together to create hierarchical categories that reflect care complexity and cost patterns.
Step 3: Score Calculation
Demographic factors combine with health status indicators to generate individual risk scores:
- Base demographic scores (age, gender, disability status)
- Condition category coefficients
- Interaction factors between multiple conditions
- Geographic and institutional adjustments
Step 4: Payment Determination
Final risk scores directly influence resource allocation and payment adjustments across healthcare organizations.
Financial Impact on Healthcare Organizations
Risk adjustment directly affects healthcare financial stability through payment accuracy and resource planning.
Paying organizations with higher-risk patient populations proportionately more ensures that they can afford to provide the treatment that patients need. Conversely, organizations serving healthier populations receive appropriate baseline payments.
Revenue Optimization Benefits
Accurate risk adjustment creates several financial advantages:
- Predictable revenue streams based on patient complexity
- Reduced financial penalties for serving high-risk populations
- Improved budget planning and resource allocation
- Enhanced ability to invest in specialized care programs
By removing the financial barrier to treating sicker patients, risk adjustment promotes fair access to healthcare for all groups.
Technology Integration in Risk Adjustment
Modern healthcare requires sophisticated technology platforms to manage complex risk adjustment processes effectively.
Digital health platforms create comprehensive patient profiles by integrating multiple data sources:
- Medical records and electronic health records (EHRs)
- Insurance claims and billing data
- Laboratory results and diagnostic reports
- Pharmacy records and prescription histories
- Patient-generated device information
In order to ensure full risk capture in accordance with MEAT (Monitor, Evaluate, Assess, Treat) standards, advanced natural language processing technology examines clinical notes to find unrecorded problems.
| Data Source | Risk Adjustment Value |
| EHR/EMR Records | Primary diagnosis capture |
| Claims Data | Historical utilization patterns |
| Lab Results | Condition severity indicators |
| Pharmacy Data | Medication adherence tracking |
| Device Data | Real-time health monitoring |
Challenges in Risk Adjustment Implementation
Healthcare organizations face several obstacles when implementing effective risk adjustment strategies.
Documentation Gaps
Incomplete medical documentation leads to understated risk scores and reduced payments. Many conditions go undocumented despite active patient management, creating significant revenue losses.
Coding Accuracy Issues
Incorrect or incomplete diagnostic coding results in:
- Missed HCC opportunities
- Inaccurate risk score calculations
- Reduced payment adjustments
- Compliance audit risks
Data Integration Complexity
Healthcare organizations often struggle with:
- Multiple disconnected data systems
- Inconsistent data formats across platforms
- Limited real-time data access
- Complex patient matching across records
Regulatory Compliance and Audit Preparation
Risk adjustment models in healthcare operate under strict regulatory oversight, requiring continuous compliance monitoring.
The Risk Adjustment Data Validation (RADV) audit process examines documentation supporting reported diagnoses. Organizations must maintain comprehensive medical records that substantiate all risk adjustment claims.
RADV Audit Requirements
Healthcare organizations must demonstrate:
- Complete medical record documentation
- Appropriate MEAT criteria application
- Accurate diagnostic code assignment
- Proper condition hierarchy management
- Timely data submission processes
Note: Effective audit preparation reduces financial penalties and maintains program integrity across all risk adjustment models.
Takeaway
Risk adjustment models are the financial foundation of healthcare, ensuring resources are distributed fairly across patient groups and populations. Accurate risk adjustment is becoming more and more important for long-term operations and high-quality patient outcomes as healthcare continues to shift toward value-based care.
At the point of care, Persivia provides complete platforms that easily connect all of your healthcare data sources, offering HCC potential and real-time insights. Across CMS-HCC, CDPS, and HHS-HCC models, our cutting-edge technology evaluates clinical notes, finds documentation gaps, and guarantees adherence to the most recent regulatory standards.